The international medical community was turned upside down in 1895. German physicist Wilhelm Röntgen was researching the electric discharge process in diluted gas when he stumbled upon a new kind of ray. He discovered its potential medical use when he made an image of his wife’s hand on a photographic plate. (When she first saw the picture, she purportedly said: “I have seen my death.”) In January 1896, Vienna’s daily newspaper, Die Presse, published Röntgen’s findings under the headline: “A Sensational Discovery.” It was sensational. It was the birth of the X-ray.
The idea of being able to see inside a live body transformed the medical profession. Today, we are in the middle of another chapter in the history of radiology.
Leading this global change is Dr. Frank Rybicki, Chief of Medical Imaging at The Ottawa Hospital (TOH) and Professor and Chair of Radiology at the University of Ottawa. In 2011, he was part of a Boston-based medical team that used 3D printing to guide North America’s first face transplant. His role at TOH is fairly new, having arrived only 18 months ago.
“One of the things I was charged to do was advance my department, and the institution as a whole. Having a 3D printing program puts Medical Imaging at the center of radiology’s international stage, moves us closer to becoming a top 10 per cent hospital in North America, and it enables Tender Loving Research by bringing new technologies to Ottawa and the region,” he explains. “3D printing is the fastest growing technology in the medical sector today, with multidisciplinary opportunities as the field evolves before us.”
3D printing was invented in 1983 and was first proposed for medical use in the late 1980s. Proponents were well ahead of their time.
“The evolution is very comparable to MRI 15 years ago when I completed my residency, in that the technology had to catch up. Now the technology can meet medical needs with enormous opportunities,” explains Dr. Rybicki.
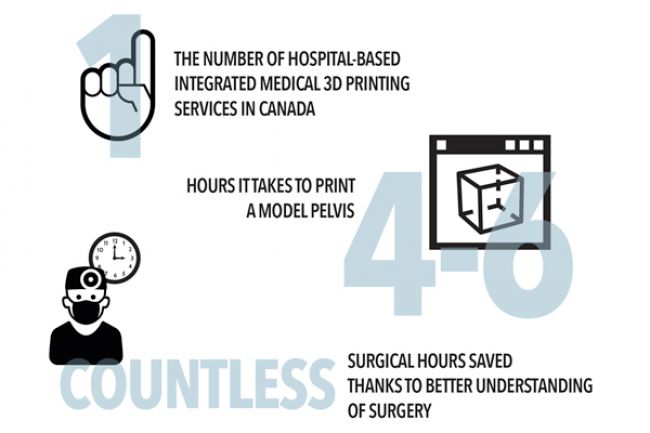
The Ottawa Hospital is the first hospital in Canada to have an integrated medical 3D printing program for surgical planning, education, and expansion of its research portfolio. It’s the kind of innovation that is helping patients today, and in the future.
Dr. Adnan Sheikh, Medical Director for 3D printing at TOH, explains its important role in complex operations.
Imagine an aggressive tumor that erodes a pelvic bone so completely that the damage extends into the joint itself. It’s a rare case and there’s a lot going on: the bone, blood vessels, muscle and soft tissues are involved. A surgeon while planning a complex surgery would like to know: 1. What’s the relationship between the tumor to the vessels? 2. What’s the best surgical approach?
3D printing can help answer these questions. Currently, this technology is widely used to create detailed anatomical models that allow doctors to plan and practice complicated heart, brain and reconstructive surgeries. These models give doctors an unprecedented level of reassurance, confidence, and clarity in complex surgeries.
The new printer allows medical staff to create a 3D replica of the damaged bone. A second model – printed to scale – shows the exact place to make critical incisions.
“Even a millimetre here or there makes a difference,” says Dr. Sheikh, who points out that having this kind of detailed information before surgery can cut operating time by two or three hours. Each hour in the operating room has a price tag of $3,000 to $4,000. Less time in the O.R. results in better patient outcomes with fewer complications during surgery.
“You know exactly what you’re doing,” says Dr. Sheikh. “That really cuts down the morbidity and any complications relating to any complex procedure.”
3D printing is also critical to research and teaching. By having models printed in 3D, the entire medical community – from students to surgeons – can benefit; not to mention the patients. Take, for example, the heart.
“Some of the abnormalities of the heart are very rare – 1/1000 or 100,000. A cardiac surgery resident may not see all the congenital heart abnormalities during their training,” says Dr. Sheikh. “How do they operate? If we had these models made so the surgeons can practice, they’d know exactly what they need to do before the surgery.”
Not too far in Ottawa’s future is a 3D printer that prints customized human implants. In the case of the patient with the tumor that destroyed his pelvic bone, imagine a 3D print of a custom prosthetic bone fragment that can safely replace the damaged one.
“3D Printing is the fastest growing technology in the medical sector today, with multidisciplinary opportunities as the field evolves before us.”
— Dr. Frank Rybicki, Chief of Medical Imaging at The Ottawa Hospital (TOH) and Professor and Chair of Radiology at the University of Ottawa.
“The technology already exists,” says Dr. Rybicki. “It’s just a matter of funding in order to bring it to Ottawa.”
Funding issues aside, the future of the 3D medical imaging program at The Ottawa Hospital looks very bright, indeed. Dr. Sheikh is particularly excited about organ printing, which would alleviate the chronic shortage of organs needed for research and transplants.
“The U.S. has already spent billions of dollars for research on organ printing and we would love to take the initiative. We have the leadership and the expertise here. That’s our aim. That’s going to change everything,” says Dr. Sheikh.
“What we are doing right now is really just the tip of the iceberg. 3D printing is revolutionizing the way we practice medicine, now, and 10 years from now.”
To find out more on how you can support The Ottawa Hospital visit ohfoundation.ca
This is part of an ongoing series about The Ottawa Hospital. Look for the evolving archive on obj.ca.

